A good friend just pointed me to an interesting article from the New York Times that came out Christmas Eve Day.
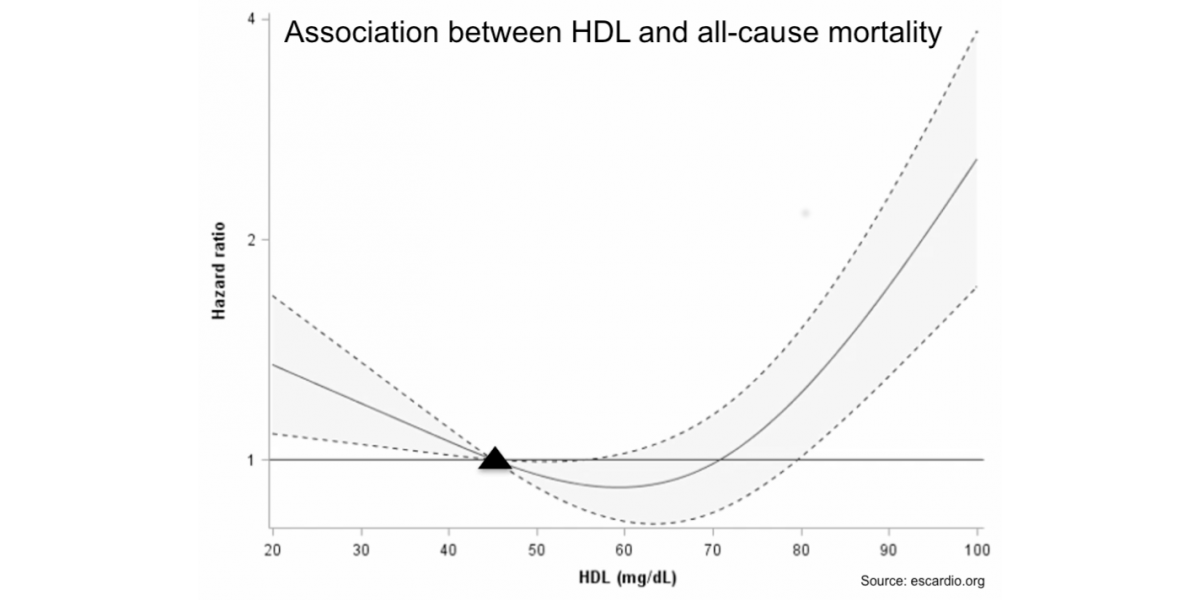
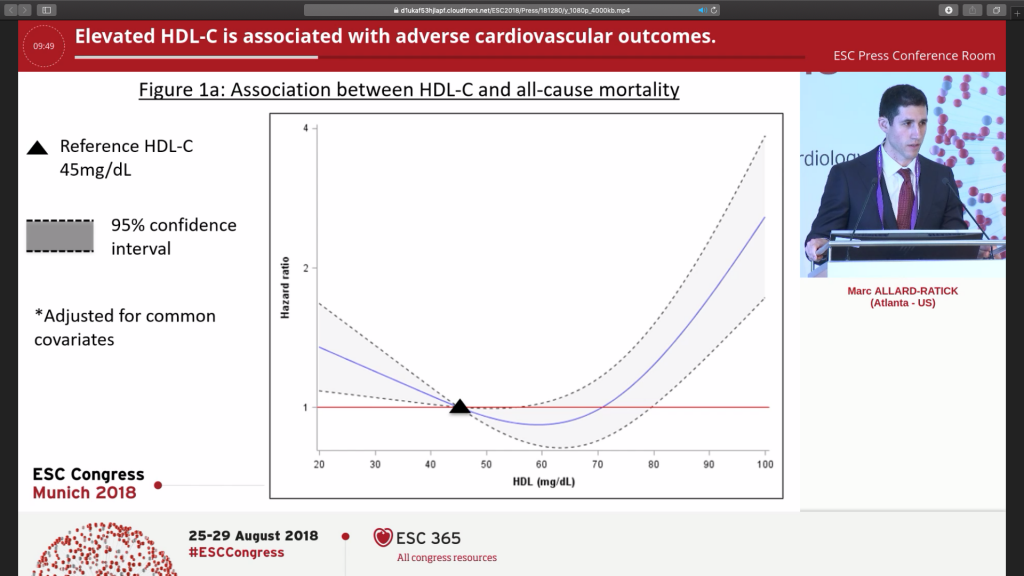
It was based on a study out of Emory University in Atlanta that showed higher all-cause mortality associated with HDL levels above 80! Below is a screen capture from the press conference where the study results were presented showing “U curve” associated with adverse events with both low HDL (<40 mg/DL) and very high HDL (>80 mg/DL).
The authors acknowledge some limitations of the study. The study started with patients that already had severe heart disease and speculate there may be some reverse causation. They also recognize that genetic mutations may be at play, citing LIPG, SCARB1, and CETP (which mean nothing to me right now!)
The recommendations were very nuanced.
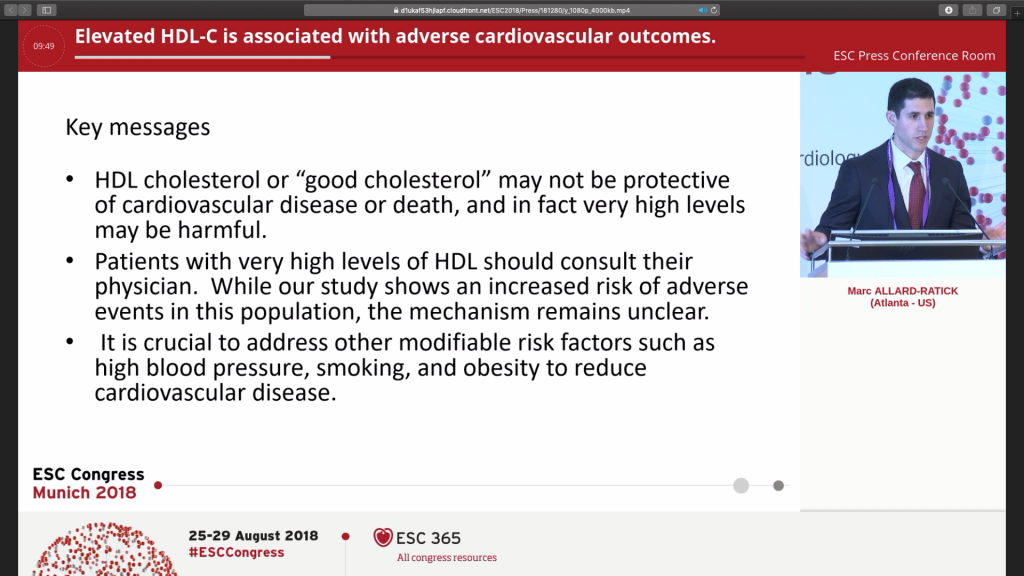
Because the mechanisms remain unclear as to why high HDL levels are associated with adverse events, they recommend focusing on the mechanisms we do know about! Still, this is the first data point I’ve seen speculating that HDL might not be protective at very high levels. This will be very interesting data to watch going forward!
The video of the press conference is accessible here.