Those of you who read this blog regularly already know that my answer would be “No! Cheese is not the enemy!” At home, we’ve chosen largely an ovo-lacto vegetarian diet, which basically means we eat eggs and cheese. But isn’t cheese the enemy?
Recent News
This topic hit my social media feed recently, so I thought I’d share my more detailed commentary!
The New York Times post covered the PURE study published in The Lancet analyzing data across 21 countries from 5 continents. Whole-fat dairy consumption of three servings per day was associated with lower rates of cardiovascular disease and mortality, compared to lower levels of consumption.
Longer History
This is simply a reinforcement of what was known from the time before I was even diagnosed with diabetes. The CARDIA study results published in 2002 actually showed an inverse relationship between dairy consumption and insulin resistance syndrome (IRS).
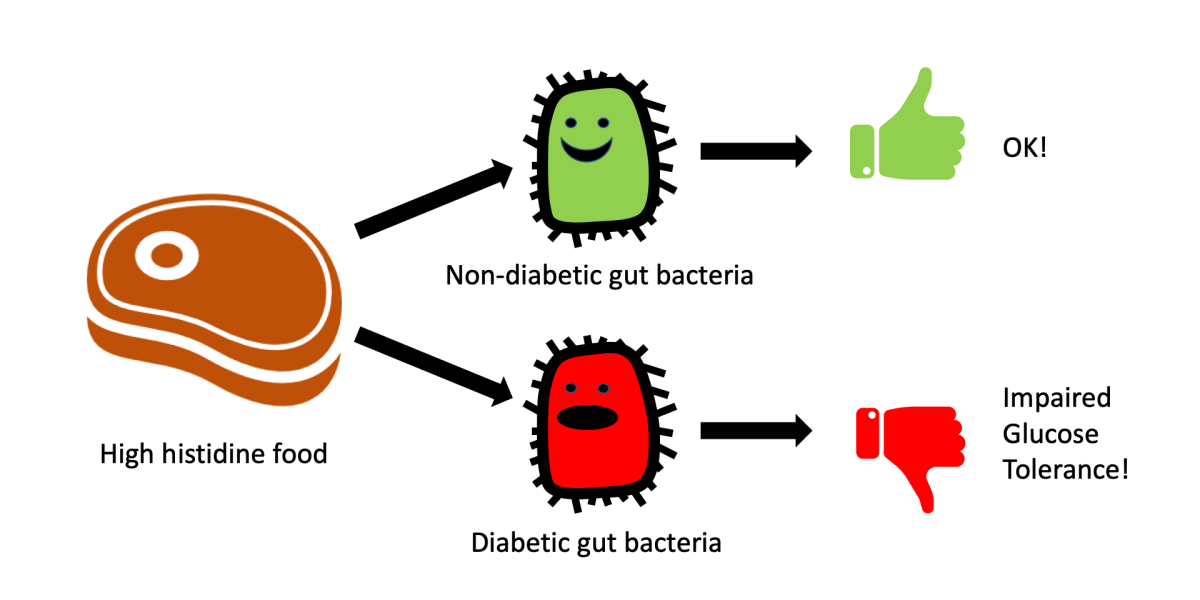
A later study in 2015 clarified that it is high-fat dairy that has the protective effects. More surprisingly, high fat dairy uniquely reduces diabetes risk but meat intake actually increases diabetes risk!
Decreased T2D [Type 2 Diabetes] risk at high intake of high- but not of low-fat dairy products suggests that dairy fat partly could have contributed to previously observed protective associations between dairy intake and T2D. Meat intake was associated with increased risk independently of the fat content.
I never bought the arguments against cheese because it is high in fat, as numerous reports — including earlier results from the PURE study — have shown that dietary fat is not associated with either cardiovascular disease or mortality. Also, I never bought the high cholesterol arguments against cheese, as high “bad” cholesterol levels appear to be unrelated to the risk of disease. Despite what our doctors are telling us, most scientists are quick to point out that our bodies are much more complex than drain pipes and that arteries don’t get clogged simply because we eat foods higher in fat and cholesterol!
The more complex issue is about the high salt content in cheese. I actually do agree with the assertion that most of us in the United States should reduce salt intake. However, a study out of Penn State showed that the sodium levels in cheese do not affect the body the way the same sodium levels do in other salty foods.
Cheese and Gut Bacteria
I happen to believe that future studies will look further into the effects of cheese on our gut bacteria. If you haven’t seen them yet, I recommend you read my posts on gut bacteria and diabetes and on gut bacteria and the metabolism of histidine.
Time wrote a very approachable piece about the potential benefits of cheese on the gut bacteria and the lower levels of the TMAO when metabolizing choline. As referenced before in a previous post, there is an association between TMAO and Type 2 diabetes, so lowering TMAO may be an indication of a protective effect in the gut!
Science will ultimately catch up here.
The Environment
Until science does catch up, there’s another more point to make here. Eating cheese does have an environmental impact. Cheese ranks 3rd highest among common foods in greenhouse gas emissions on a per kilogram basis — higher than pork and chicken — largely because of the amount of milk it takes to make cheese.
Less dense cheeses and younger cheeses, such as cottage cheese, feta, brie, or camembert, don’t use as much milk and thus have a lower environmental impact. It’s also important to note in most cultures, cheese is not eaten in large quantities. It may be common in many cultures to eat a big piece of meat with a meal, but it’s not as common to eat a whole wheel of cheese at once!
For environmental reasons — independent of health considerations — try not to overindulge in cheese, and also be sure to eat what you buy!
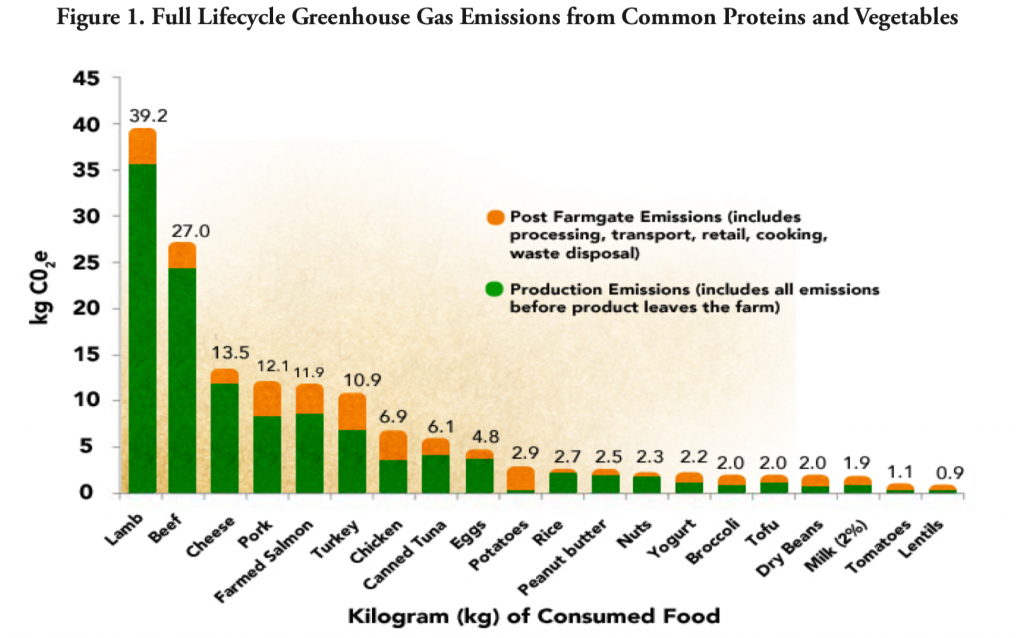
Photo by Tabitha Mort from Pexels